|
Odontogenic cyst
Odontogenic cysts are a group of jaw cysts that are formed from tissues involved in odontogenesis (tooth development). Odontogenic cysts are closed sacs, and have a distinct membrane derived from the rest of odontogenic epithelium. It may contain air, fluids, or semi-solid material. Intra-bony cysts are most common in the jaws, because the mandible and maxilla are the only bones with epithelial components. That odontogenic epithelium is critical in normal tooth development. However, epithelial rests may be the origin for the cyst lining later. Not all oral cysts are odontogenic cysts. For example, mucous cyst of the oral mucosa and nasolabial duct cyst are not of odontogenic origin. In addition, there are several conditions with so-called (radiographic) 'pseudocystic appearance' in jaws; ranging from anatomic variants such as Stafne static bone cyst, to the aggressive aneurysmal bone cyst.[1] Classification[2]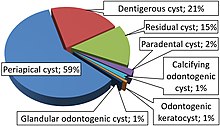
Cystic neoplasmMost cysts in the body are benign (dysfunctional) tumors, the result of plugged ducts or other natural body outlets for secretions. However, sometimes these masses are considered neoplasm:
Diagnosis On histopathology, cholesterol clefts indicate mainly a periapical (radicular) cyst[4] or an inflamed dentigerous cyst.[5] TreatmentTreatment ranges from simple enucleation of the cyst to curettage to resection. For example, small radicular cyst may resolved after successful endodontic ("root-canal") treatment. Because of high recurrence potential and aggressive behaviour, curettage is recommended for keratocyst. However, the conservative enucleation is the treatment of choice for most odontogenic cysts. The removed cyst must be evaluated by pathologist to confirm the diagnosis, and to rule out other neoplastic lesions with similar clinical or radiographic features (e.g., cystic or solid ameloblastoma, central mucoepidermoid carcinoma).[6] There are cysts, e.g. buccal bifurcation cyst with self-resolation nature, in which close observation can be employed unless the cyst is infected and symptomatic.[7] See alsoReferences
|